Stay updated on what is trending in health. Discover tips and resources for a healthier, balanced life.
What is Meningitis? What Causes It, and How to Protect Yourself
What is meningitis? Learn all about the causes, symptoms, types, treatments, and prevention strategies for meningitis in this clear, easy-to-understand guide.
DISEASES AND CONDITIONS
Dr. S. Ali
1/14/20266 min read
Meningitis is a serious and sometimes life-threatening condition that demands attention. But how much do you really know about it? Whether you've heard of it through a news story, a college campus alert, or a concerned parent, understanding meningitis could help save a life—maybe even your own.
In this article, we'll walk through what meningitis is, what causes it, its symptoms, how it spreads, the different types, who’s most at risk, and how you can prevent it.
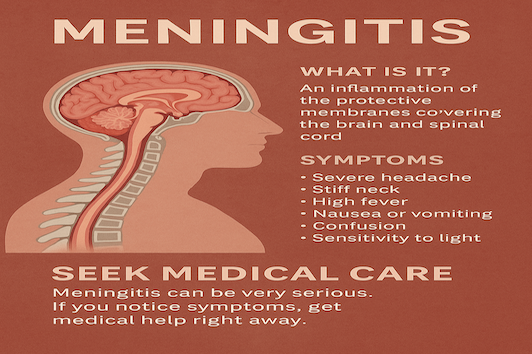
What Is Meningitis?
Meningitis is an inflammation of the meninges—the protective membranes that cover your brain and spinal cord. This inflammation is typically triggered by an infection, and it can come on quickly and progress rapidly.
Meningitis is most commonly caused by viruses and bacteria, but it can also result from fungi, parasites, cancer, autoimmune diseases, and certain medications. The specific cause affects how serious the illness is and how it’s treated.
Bacterial and viral meningitis are the most common. The bacterial form is generally more severe and can be life-threatening without prompt treatment. Viral meningitis is typically less severe than the bacterial form and often improves without specific treatment in otherwise healthy individuals — but it can still cause serious symptoms and complications, especially in vulnerable groups.
Common Symptoms of Meningitis
Meningitis symptoms can appear suddenly and worsen quickly.They often resemble the flu at first, making early diagnosis difficult. But quick recognition can save lives. Here's what to look out for:
Sudden high fever
A rapid spike in temperature is one of the earliest and most common signs. It’s your body reacting to an infection.Severe headache
This isn’t a typical headache — it’s intense and persistent, often described as unbearable.Stiff neck
Difficulty moving the neck or looking down/up without pain is a hallmark sign of meningitis.Nausea or vomiting
Often accompanies the headache and fever, especially in bacterial meningitis cases.Sensitivity to light (photophobia)
Bright lights may feel harsh or painful to the eyes, signaling irritation in the brain.Confusion or difficulty concentrating
The infection can affect brain function, leading to disorientation, slurred speech, or a foggy mind.Sleepiness or difficulty waking
This could indicate the brain is under stress. It’s especially dangerous in children and older adults.Seizures
Seizures may occur as the brain becomes inflamed — always a red flag that needs urgent care.Skin rash (especially in meningococcal meningitis)
A purple, bruise-like rash may appear and doesn’t fade when pressed. It’s a sign the infection has entered the bloodstream.
In infants and young children, watch for:
High-pitched crying
This unusual, persistent cry can indicate discomfort or neurological distress.Poor feeding
Babies may refuse to eat or seem too weak to nurse or bottle-feed.Bulging soft spot on the head (fontanel)
Swelling of the soft spot on a baby’s head may reflect pressure from brain inflammation.Irritability or lethargy
Unusual fussiness or extreme sleepiness (hard to wake) should not be ignored.If you or someone you know shows these signs, don’t wait. Meningitis can progress rapidly — seek emergency medical care immediately.
Types of Meningitis
There are several different types of meningitis. Let’s break them down:
Bacterial Meningitis
This is the most serious type. It requires immediate treatment with antibiotics and sometimes corticosteroids. Common bacteria that cause meningitis include:
Streptococcus pneumoniae
Haemophilus influenzae type b (Hib)
Listeria monocytogenes (especially in older adults and pregnant women)
How it spreads: Through respiratory droplets—coughing, sneezing, or kissing.
Prevention: Vaccines are highly effective against many of these bacteria.
Viral Meningitis
Also called aseptic meningitis, this is the most common type and generally less severe. It's usually caused by:
Enteroviruses
Herpes simplex virus
Mumps virus
How it spreads: Close contact, poor hygiene, and respiratory droplets.
Treatment: Most people recover on their own in 7–10 days. Fluids, rest, and pain relievers are usually enough.
Fungal Meningitis
Fungal meningitis occurs when fungi spread from another part of the body to the brain or spinal cord. It’s most commonly caused by a fungus called Cryptococcus, especially in people with weakened immune systems (such as those with HIV/AIDS, cancer, or on immunosuppressive drugs).
How it spreads: Typically not from person to person. You can inhale fungal spores from the environment.
Treatment: Requires long-term antifungal medications.
Parasitic
Parasitic meningitis is rare, but when it does occur, it’s often due to specific parasites like:
· Naegleria fowleri (the “brain-eating amoeba”) — found in warm freshwater lakes and hot springs. Causes a very aggressive infection called Primary Amebic Meningoencephalitis (PAM), which is almost always fatal.
· Other parasites may cause eosinophilic meningitis, which can result from eating contaminated food (like raw snails or undercooked fish).
Non-Infectious Meningitis: When Infection Isn’t the Cause
Unlike viral or bacterial meningitis, non-infectious meningitis isn’t caused by germs. Instead, it’s triggered by other factors, including:
Autoimmune Diseases:
Conditions like lupus or sarcoidosis can cause the immune system to mistakenly attack the membranes around the brain and spinal cord.Cancers:
Certain cancers, especially those that spread to the brain (like leukemia or lymphoma), can lead to meningitis-like inflammation.Head Injuries:
Trauma to the head can irritate the meninges (protective layers around the brain), leading to inflammation without infection.Medications:
Some drugs—such as NSAIDs, antibiotics, or intravenous immunoglobulins—can trigger an inflammatory response that mimics meningitis.Post-Surgical Inflammation:
Brain or spinal procedures may cause sterile (non-infectious) inflammation as a side effect.
While non-infectious meningitis doesn’t spread from person to person, it can still cause inflammation and symptoms similar to infectious meningitis — such as headache, neck stiffness, and fever — and requires proper diagnosis and management based on the underlying cause.
Who Is Most at Risk?
Meningitis can affect anyone, but certain groups are more vulnerable:
Infants and young children
Teenagers and young adults, especially in dorms or military housing
Elderly adults
People with weakened immune systems
Travelers to areas where meningitis is more common (e.g., parts of Africa)
How Is Meningitis Diagnosed?
Doctors use several methods to confirm meningitis:
Lumbar puncture (spinal tap): To test cerebrospinal fluid for infection.
Blood cultures: To identify the organism causing the infection.
Imaging: MRI or CT scan to detect brain swelling.
Getting diagnosed quickly is critical for survival, especially for bacterial meningitis.
How Is Meningitis Treated?
Treatment depends on the type:
Bacterial meningitis: Intravenous (IV) antibiotics and sometimes steroids.
Viral meningitis: Usually supportive care—hydration, rest, and over-the-counter medications.
Fungal meningitis: Antifungal medications over several weeks.
Parasitic meningitis: Often has no effective treatment, but symptoms may be managed.
Non-infectious meningitis: Treat the underlying cause (e.g., stopping a medication or managing autoimmune disease).
In severe cases, patients may require hospitalization and close monitoring for complications like seizures, hearing loss, or brain damage.
Can Meningitis Be Prevented?
Absolutely! Here’s how you can reduce your risk:
This is the number one way to prevent certain types of meningitis. Key vaccines include:
Meningococcal vaccine: Especially for teens, college students, and travelers
Pneumococcal vaccine: For infants, older adults, and people with chronic conditions
Hib (Haemophilus influenzae type b) vaccine: Given in early childhood
MMR (Measles, Mumps, Rubella): Prevents viruses that can lead to meningitis
Practice Good Hygiene
Wash hands regularly
Don’t share utensils, drinks, or toothbrushes
Cover coughs and sneezes
Boost Your Immune System
Eat a balanced diet, stay active, and get enough sleep to help your body fight off infections.
Know When to Seek Help
The earlier you get treatment, the better the outcome. Don’t ignore the signs.
FAQs About Meningitis
Q: Is meningitis contagious?
A: Yes, some forms—like bacterial and viral meningitis—can spread through respiratory droplets. That’s why close living environments (like college dorms) are common outbreak spots.
Q: How quickly does meningitis progress?
A: Bacterial meningitis can become life-threatening in hours. That’s why rapid treatment is so important.
Q: Can you get meningitis more than once?
A: Yes, it’s rare but possible. Your immune system may not always build full protection, especially if the cause is a different virus or bacteria.
Q: Is there a test I can take at home?
A: No. Meningitis requires professional diagnosis through tests like a spinal tap and blood work.
Q: What should I do if I think I or someone else has meningitis?
A: Go to the emergency room immediately. This is not something to “wait and see” about.
Q: Is viral meningitis always mild?
A: Not always. While viral meningitis is often less severe than bacterial meningitis, it can still cause serious complications in young children, older adults, and people with compromised immune systems.
Q: How long does it take to recover from meningitis?
A: Recovery time depends on the type and severity. Mild viral meningitis may resolve in 7–10 days, while bacterial meningitis can lead to longer hospital stays and ongoing complications like hearing loss or memory problems.
Q: Can meningitis cause long-term problems?
A: Yes. Some survivors may experience lasting effects such as hearing loss, vision problems, cognitive difficulties, or seizures—especially if treatment is delayed.
Final Thoughts
Meningitis may be rare, but it’s not something to take lightly. Its rapid onset and potential for life-altering complications make awareness, prevention, and early treatment critical.
If you're eligible for a vaccine—get it. If you're a parent—make sure your kids are protected. If you're experiencing suspicious symptoms—don’t wait. Trust your instincts and seek help.
Knowing the signs and understanding your risk could make all the difference.
Related Articles:
1. Invasive Meningococcal Disease (IMD): What You Need to Know
2. Brain-Eating Amoeba: Risks & Symptoms of Naegleria Fowleri
Sources
1. Centers for Disease Control and Prevention (CDC)
https://www.cdc.gov/meningitis/index.html
2. World Health Organization (WHO)
https://www.who.int/health-topics/meningitis
3. Meningitis Research Foundation (UK)
https://www.meningitis.org/
4. Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/meningitis/symptoms-causes/syc-20350508
5. National Institute of Neurological Disorders and Stroke (NINDS - NIH)
https://www.ninds.nih.gov/health-information/disorders/meningitis
6. Johns Hopkins Medicine
https://www.hopkinsmedicine.org/health/conditions-and-diseases/meningitis
Pulse Your Health
Empowering you to achieve your health goals.
Contact
© 2026. All rights reserved.
Disclaimer: The content on this website is for informational purposes only and is not medical advice. Always seek the advice of your physician or other suitably qualified healthcare professional for diagnosis, treatment and your health related needs.
