Stay updated on what is trending in health. Discover tips and resources for a healthier, balanced life.
What Happens If Your Bladder Is Removed?
Wondering what life is like after bladder is removed? Learn about recovery, daily routines, intimacy, travel, diet changes, and long-term health tips—all in a supportive, conversational guide.
SURGERIES
Dr. S. Ali
7/30/20255 min read
What Happens If Your Bladder Is Removed?
Living Without a Bladder: What You Need to Know
Did your doctor mention bladder removal—or maybe you’ve heard the term cystectomy—and now you’re wondering, “How do people live without a bladder?” You’re not alone. It sounds scary, but thousands of people live full lives after bladder removal. Here’s what really happens, in plain English.
Why Would Someone Need Their Bladder Removed?
The most common reason is bladder cancer—especially if it’s invasive or recurrent. But a bladder might also be removed due to:
Trauma or injury
Severe bladder dysfunction or birth defects
Chronic interstitial cystitis (in rare, extreme cases)
So… What Happens When the Bladder Is Gone?
Your bladder’s job is to store urine until it’s time to go. When it’s removed, your body still makes urine—it just needs a new way to get rid of it.
That’s where urinary diversion comes in. There are a few options, depending on your health, lifestyle, and doctor’s recommendation.
1. Urostomy (Ileal Conduit)
This is the most common method. Here’s how it works:
A piece of your small intestine is used to create a passage for urine to exit your body.
Urine flows from your kidneys through this tube and exits through a small opening (called a stoma) on your abdomen.
It collects in an external urostomy bag that sticks to your skin.
“Will people see it?”
Urostomy bags are discreet and fit under clothing. With practice, most people manage them easily.
2. Neobladder (New Bladder)
Some people are candidates for a neobladder, which is a new bladder made from a piece of intestine.
It’s connected to your urethra, so you can pee more normally.
You may need to learn how to use abdominal muscles to help empty it.
In some cases, people have to use a catheter to make sure it’s fully drained.
“Will I feel the urge to go?”
Sometimes yes, but many people lose the typical sensation. You’ll often go on a schedule at first.
3. Continent Reservoir (Indiana Pouch)
This is a pouch created inside the body using a section of intestine.
It stores urine and connects to a stoma.
Instead of using a bag, you insert a catheter into the stoma to empty it a few times a day.
“Is it hard to do?”
It takes getting used to, but many find this option gives them more control.
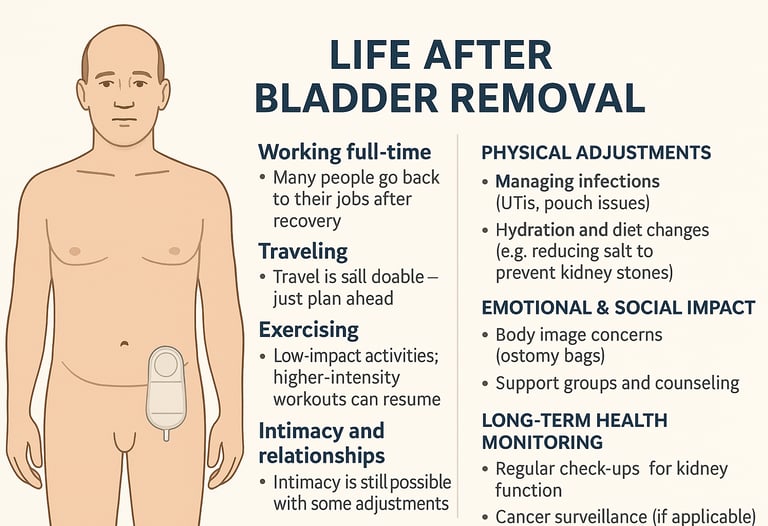
What’s Life Like After Bladder Removal?
It definitely takes some adjustment, but most people return to a full and satisfying life. Here’s how things typically go:
Working full-time
Many people go back to their jobs after recovery. You might need a few weeks or months off depending on your surgery type, but long-term, your career doesn’t have to take a back seat.Traveling
Travel is still totally doable! Just plan ahead—pack extra urostomy supplies or catheters, and map out restroom stops. With a little preparation, you can go anywhere.Exercising
Staying active is encouraged. Low-impact activities like walking, yoga, or swimming are great during recovery. Once you're cleared, even running, cycling, or strength training may be back on the table.Intimacy and relationships
It’s natural to feel nervous at first, but intimacy is still very possible. Open communication with your partner, emotional support, and sometimes medical advice can help restore confidence and connection.
Physical Adjustments
Managing infections
Urinary tract infections (UTIs) and pouch-related issues can happen. Practicing good hygiene, drinking plenty of water, and addressing symptoms early are key to preventing complications.Hydration and diet changes
After bladder removal, staying hydrated is essential to protect your kidneys. You may need to reduce salt intake and limit certain foods to prevent kidney stones or digestive upset (especially if intestines were used in reconstruction).
Emotional & Social Impact
Body image concerns
If you have a stoma or external pouch, it can take time to adjust. It’s normal to feel self-conscious at first, but most people adapt—and many devices are now discreet and user-friendly.Support groups and counseling
Talking with others who’ve been through it can make a world of difference. Whether it’s an in-person group or online forum, support can help you process emotions and regain confidence.
Long-Term Health Monitoring
Regular check-ups for kidney function
Your kidneys still filter waste, and regular monitoring ensures they’re staying healthy—especially if you have a urinary diversion that uses bowel tissue.Cancer surveillance (if applicable)
If your bladder was removed due to cancer, ongoing surveillance is important. Your healthcare provider may recommend periodic imaging, bloodwork, or cytology to catch any recurrence early.
What This Means for You
Life after bladder removal can be full and active—most patients resume work, travel, and routines within a year.
The type of urinary diversion matters for convenience, body image, and emotional well‑being—but personal choice and medical guidance are key.
Robotic surgery shows promise for smoother recovery, but both surgical approaches deliver comparable survival.
As always, personalized care, strong surgical teams, and realistic expectations shape outcomes.
Are There Any Side Effects or Risks?
Yes, as with any major surgery. These can include:
Infections
Any surgery carries a risk of infection—especially around the surgical site or urinary tract. Good hygiene and prompt treatment are key to recovery.Urine leaks or blockage
If the new urinary pathway doesn’t function smoothly, leaks or blockages can occur. These may require minor procedures or catheter use.Bowel changes (especially if intestines are used)
When part of the intestine is used to create a urinary diversion, it can lead to digestive changes like diarrhea, gas, or absorption issues.Stoma care issues
If you have a urostomy, learning to manage the stoma and pouching system takes time. Skin irritation or pouch leaks may happen early on.Emotional and body image adjustments
Coping with physical changes—like a stoma or new bathroom habits—can affect confidence and mental health. Counseling or support groups can be a big help.
Are There Alternatives to Bladder Removal?
While radical cystectomy remains standard for muscle-invasive bladder cancer, bladder-preserving strategies are being studied—especially for non-muscle-invasive disease:
Intravesical therapy: Treatments placed directly into the bladder—like chemotherapy or immunotherapy may help some patients avoid bladder removal, especially in early-stage cancers.
Trimodality therapy (TMT): A combination of surgery to remove the tumor, followed by chemotherapy and radiation, is being explored as a way to treat cancer while keeping the bladder intact.
In short: bladder removal is evolving. Modern surgical techniques and personalized diversion choices can help preserve quality of life. And for some patients, bladder‑preserving therapies may be a viable path—especially in earlier cancer stages.
Final Thoughts: You’re Not Alone
If you or a loved one is facing bladder removal, it’s normal to feel overwhelmed. But with the right care and information, you can live a full, active life. There are support groups, medical teams, and real people out there ready to help.
Sources:
BMC Cancer (2024) – Continence outcomes and satisfaction after robotic-assisted radical cystectomy with Mainz pouch II
https://bmccancer.biomedcentral.com/articles/10.1186/s12885-024-11874-xMemorial Sloan Kettering Cancer Center – Patients with bladder cancer report favorable long-term quality of life after radical cystectomy
https://www.mskcc.org/clinical-updates/patients-bladder-cancer-report-favorable-long-term-quality-life-after-radical-cystectomyPubMed (2024) – Emotional functioning six years after radical cystectomy: A long-term prospective study
https://pubmed.ncbi.nlm.nih.gov/39947291ASCO Journals (2024) – Trends in early mortality and postoperative complications after radical cystectomy in the US
https://ascopubs.org/doi/10.1200/JCO.2024.42.4_suppl.583Urology Times (2023) – Robotic cystectomy shows noninferior long-term OS vs open cystectomy
https://www.urologytimes.com/view/robotic-cystectomy-shows-noninferior-long-term-os-vs-open-cystectomy-in-urothelial-carcinomaNational Cancer Institute – Bladder Cancer Treatment (PDQ®)
https://www.cancer.gov/types/bladder/patient/bladder-treatment-pdqJohns Hopkins Medicine – Radical Cystectomy Overview
https://www.hopkinsmedicine.org/health/conditions-and-diseases/bladder-cancer/radical-cystectomy
Pulse Your Health
Empowering you to achieve your health goals.
Contact
© 2026. All rights reserved.
Disclaimer: The content on this website is for informational purposes only and is not medical advice. Always seek the advice of your physician or other suitably qualified healthcare professional for diagnosis, treatment and your health related needs.
