Stay updated on what is trending in health. Discover tips and resources for a healthier, balanced life.
Valley Fever: What You Need to Know About This Dusty Danger
Valley Fever (coccidioidomycosis) is a fungal infection common in the U.S. Southwest. Learn its symptoms, causes, risks, and prevention tips in this easy-to-read guide.
DISEASES AND CONDITIONS
Dr. S. Ali
8/20/20256 min read
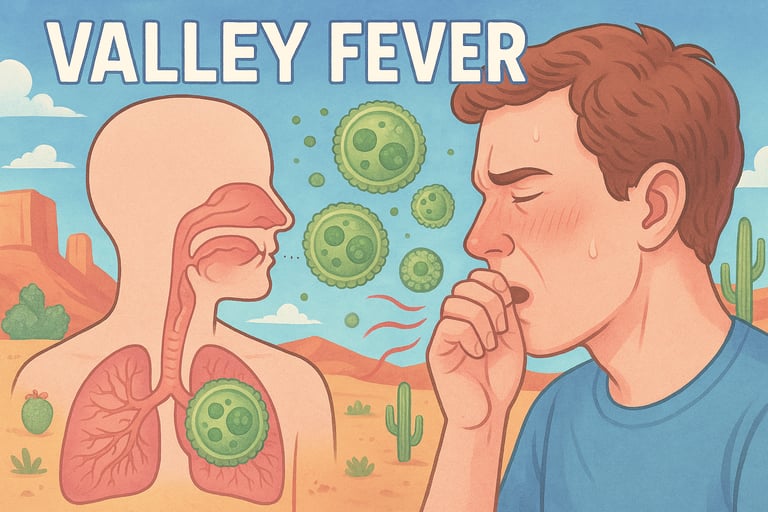
When you hear the words “Valley Fever”, you might think it’s just another seasonal bug that goes around. But in reality, Valley Fever—also called coccidioidomycosis—is a fungal infection that can cause serious illness in some people. If you live in or travel to certain parts of the U.S., particularly the Southwest, this is something worth knowing about.
What Exactly Is Valley Fever?
Valley Fever is caused by a fungus called Coccidioides, which lives in the soil. When the ground is disturbed—by farming, construction, or even a windy day—tiny fungal spores can become airborne. If you breathe them in, they can settle in your lungs and cause infection.
It’s not contagious (you can’t catch it from another person), but it spreads easily in dry, dusty environments where the fungus thrives.
Where Is Valley Fever Found?
Valley Fever is most common in the U.S. Southwest, but it’s not limited to that area. Here’s the breakdown:
The majority of cases are reported in Arizona and California, especially in Phoenix, Tucson, and California’s Central Valley.
Other states with cases include Nevada, New Mexico, Utah, and Texas, though the numbers are smaller.
The fungus (Coccidioides) thrives in dry, dusty soils, making desert climates the perfect environment for it to grow. That’s why the Southwest is considered the “hot spot.”
However, cases have also been detected outside the Southwest, including in Washington State, northern Mexico, and parts of Central and South America.
So while the Southwest U.S. remains the core region, Valley Fever is not exclusive to that area. Public health experts warn that climate change and shifting weather patterns could expand the fungus’s habitat, potentially increasing cases in places not historically known for Valley Fever.
Is Valley Fever Common in Other Countries?
While Valley Fever is best known in the U.S. Southwest, it isn’t unique to America. The fungus that causes the infection, Coccidioides, is also found in parts of northern Mexico, Central America, and South America. In these regions, the same dry, dusty soil conditions make it possible for the spores to survive.
That said, the highest number of diagnosed cases comes from the U.S., largely because of better awareness and stronger testing systems. In some Latin American countries, cases may be underreported or misdiagnosed as pneumonia or tuberculosis.
So yes, Valley Fever exists beyond U.S. borders, but it is most closely tracked and recognized in the United States.
What Are the Symptoms?
Valley Fever can look and feel a lot like the flu or a respiratory infection, which is why it sometimes gets missed. Symptoms can range from mild to severe, and in many cases, they show up a week or two after breathing in the fungal spores. Here’s what people often experience:
Fever and chills – Your body naturally raises its temperature to try and fight off the fungus, which can leave you shivering one moment and burning up the next. These episodes may come and go, much like when you have the flu.
Cough and chest pain – Because Coccidioides spores settle into the lungs, the infection often causes a persistent cough. Some people may also feel tightness or sharp pain in the chest, especially when taking a deep breath. In more severe cases, the cough can produce mucus or even blood.
Fatigue – Feeling unusually tired is one of the most common complaints. Even after other symptoms improve, fatigue may linger for weeks or months, making daily activities feel like a struggle.
Headaches and muscle aches – Valley Fever can trigger widespread aches and pains throughout the body, very similar to what you might feel during a viral illness like the flu. Headaches can be dull or throbbing, and muscle soreness often adds to the sense of being unwell.
Rash – In some cases, painful red bumps—often called “erythema nodosum”—appear on the skin, usually on the lower legs or arms. While they may look alarming, these rashes are actually a sign that your immune system is mounting a strong response against the infection.
Not everyone will experience all these symptoms, and some people may have only mild signs or none at all. But if you live in or have recently traveled to an area where Valley Fever is common, it’s worth paying attention to these warning signals.
Most healthy people recover on their own within weeks or months. But for others—especially those with weakened immune systems—the infection can become severe or even spread to other parts of the body, like the brain, skin, or bones.
Who Is Most at Risk for Valley Fever?
While anyone can breathe in the fungal spores and develop Valley Fever, certain groups of people are more likely to experience serious illness or complications. Here’s a closer look at who may be more vulnerable:
People with weakened immune systems – Your immune system is your body’s defense army, and if it’s not at full strength, it has a harder time fighting off infections. This includes people living with HIV/AIDS, those who have received organ transplants, or anyone taking immune-suppressing medications (such as steroids or chemotherapy drugs). In these cases, Valley Fever can spread beyond the lungs and cause more serious disease.
Pregnant women – Pregnancy naturally lowers parts of the immune response to help the body accept and protect the baby. Because of this, pregnant women—especially in the later stages of pregnancy—are at higher risk of developing severe Valley Fever.
Adults over 60 – As we age, our immune systems tend to become less efficient. Older adults are therefore more likely to experience complications from Valley Fever, such as chronic lung problems or long-lasting fatigue.
People of African American or Filipino descent – Research has shown that individuals from these backgrounds may face a higher risk of developing severe or disseminated (widespread) forms of Valley Fever. The reasons aren’t fully understood, but experts believe it may be linked to genetic and immune system factors.
While being in one of these groups doesn’t guarantee severe illness, it does mean that extra caution is important. If you live in or travel to areas where Valley Fever is common, knowing your risk can help you act quickly if symptoms appear.
How Is Valley Fever Diagnosed and Treated?
Because symptoms mimic the flu, Valley Fever is often misdiagnosed or overlooked. A doctor can confirm it with blood tests, chest X-rays, or fungal cultures.
Treatment depends on the severity:
Mild cases often resolve without medication.
In many healthy individuals, Valley Fever symptoms improve on their own within weeks to months, similar to recovering from a flu-like illness. Rest, hydration, and monitoring are usually all that’s needed.Moderate to severe cases may require antifungal medications like fluconazole or itraconazole.
These medications help stop the fungus from multiplying and spreading, reducing symptoms and preventing complications. Treatment may last for several months depending on how well a person responds.Chronic or disseminated infections can need long-term or even lifelong antifungal therapy.
When the infection spreads beyond the lungs—such as to the skin, bones, or brain—ongoing treatment is often necessary to keep the fungus under control. In some cases, lifelong monitoring and medication are essential to prevent relapses.
Can You Prevent Valley Fever?
There’s no vaccine yet, but you can lower your risk if you live in or travel to high-risk areas:
Avoid activities that stir up a lot of dust (especially on windy days).
Digging, gardening, or construction work can release fungal spores into the air. If possible, postpone these activities when the soil is dry and winds are strong.Wear an N95 mask when working outdoors in dusty conditions.
A properly fitted N95 mask can significantly reduce the chance of inhaling spores. This is especially important for farmers, construction workers, and anyone spending long hours outside in endemic areas.Keep doors and windows closed during dust storms.
This simple step helps prevent spores from entering your home and settling on surfaces. Using air purifiers indoors can add an extra layer of protection.Stay informed if you live in endemic regions—health departments often issue warnings during peak seasons.
Local alerts can help you take precautions, like limiting outdoor exposure when the risk is highest. Staying aware ensures you’re ready to protect yourself and your family.
Valley Fever and Climate Change
Here’s something worth noting: researchers believe Valley Fever may spread to new areas as rising temperatures and droughts create more suitable environments for the fungus. This means more people—even outside the Southwest—could be exposed in the future.
The Bottom Line
Valley Fever might sound like a regional health issue, but it’s one that’s gaining attention nationwide. If you’ve recently traveled to the Southwest and develop a lingering cough, fatigue, or flu-like symptoms that just don’t go away—don’t ignore it. Talk to your doctor and ask about Valley Fever.
Staying aware and informed is your best defense.
Sources:
Centers for Disease Control and Prevention (CDC)
https://www.cdc.gov/valley-fever/index.htmlMayo Clinic
https://www.mayoclinic.org/diseases-conditions/valley-fever/symptoms-causes/syc-20378761CDC
https://www.cdc.gov/valley-fever/hcp/clinical-overview/index.htmlCDC Yellow Book
https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/coccidioidomycosis-valley-feverCalifornia Department of Public Health
https://www.cdph.ca.gov/valleyfeverCleveland Clinic
https://my.clevelandclinic.org/health/diseases/17754-valley-fever
CDC
https://www.cdc.gov/valley-fever/php/statistics/index.htmlWashington Department of Health
https://doh.wa.gov/you-and-your-family/illness-and-disease-z/valley-fever-coccidioidomycosisUniversity of Arizona
https://vfce.arizona.edu/valley-fever-people/about-valley-fever
Pulse Your Health
Empowering you to achieve your health goals.
Contact
© 2026. All rights reserved.
Disclaimer: The content on this website is for informational purposes only and is not medical advice. Always seek the advice of your physician or other suitably qualified healthcare professional for diagnosis, treatment and your health related needs.
