Stay updated on what is trending in health. Discover tips and resources for a healthier, balanced life.
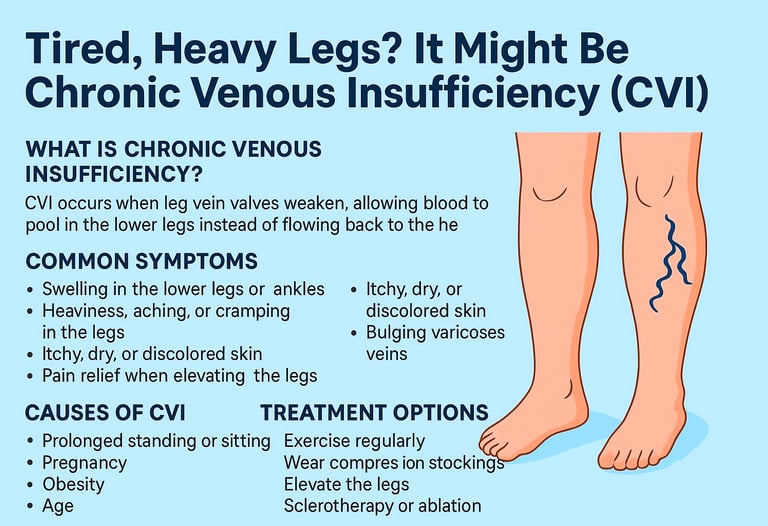
Tired, Heavy Legs? It Might Be Chronic Venous Insufficiency (CVI)
Discover what Chronic Venous Insufficiency (CVI) is, why it occurs, and how to treat it. Explore symptoms, risk factors, and prevention tips in one easy guide
DISEASES AND CONDITIONS
Dr. S. Ali
8/26/20256 min read
Ever feel like your legs are heavy, achy, or swollen—especially at the end of the day? It might not just be fatigue. You could be dealing with chronic venous insufficiency (CVI), a condition that affects millions of people but often flies under the radar.
Let’s break it down in simple terms—what chronic venous insufficiency (CVI) is, why it happens, and what you can do about it.
What Is Chronic Venous Insufficiency?
chronic venous insufficiency (CVI) happens when the veins in your legs don’t work as they should. Normally, veins have one-way valves that help push blood back up toward your heart. But when these valves become weak or damaged, blood can pool in your legs instead of moving upward. This leads to symptoms like:
Swelling in the lower legs or ankles
This is often worse at the end of the day and may make your shoes feel tight or uncomfortable.A feeling of heaviness, aching, or cramping
Your legs might feel like they're dragging, especially after standing or sitting for long periods.Itchy, dry, or discolored skin
Skin around the ankles may become irritated, flaky, or take on a reddish-brown hue over time.Bulging varicose veins
These twisted, rope-like veins are a common sign that blood isn’t flowing properly.Pain that improves when you raise your legs
Elevating your legs helps blood drain back toward the heart, easing discomfort and swelling.
Over time, if left untreated, chronic venous insufficiency (CVI) can cause skin changes, ulcers, and serious complications.
What Causes It?
Several factors can put extra strain on your leg veins:
Prolonged standing or sitting
Jobs that keep you on your feet (or in a chair) for hours can interfere with healthy blood flow. Without regular movement, blood tends to pool in the legs, making it harder to circulate upward.Pregnancy
The growing uterus adds pressure to your veins and increases blood volume. Hormonal changes during pregnancy also relax vein walls, which can further slow circulation.Obesity
Extra weight puts stress on your legs and veins. It increases pressure inside the veins, which can stretch and damage the delicate valves.Age
As we get older, our veins and valves naturally weaken. This makes it more difficult for them to function properly and keep blood flowing in the right direction.Family history
If your parents had vein issues, you’re more likely to have them too. Genetics can affect vein structure and valve strength, making you more prone to chronic venous insufficiency (CVI).Previous blood clots or vein damage
These can impair blood flow and damage vein valves permanently. Once valves are damaged, they can’t close properly, leading to backward blood flow and pooling.
How Do You Know If You Have It?
Chronic venous insufficiency (CVI) symptoms often develop slowly, so many people shrug them off for years. You might chalk it up to “just tired legs” or “poor circulation,” but early diagnosis is key.
Watch for:
Leg swelling that gets worse by evening
You may notice your socks or shoes feeling tighter as the day goes on. This swelling usually improves overnight as you lie down, letting gravity help your veins.Skin that feels tight or looks shiny
As fluid builds up, the skin over your lower legs may stretch and lose its natural texture. It can feel uncomfortable, like your skin is under pressure.Brownish or reddish discoloration around the ankles
This staining happens when blood leaks from weakened veins and breaks down under the skin. It’s often a sign that CVI has been going on for a while.Varicose veins that seem to multiply
These twisted, bulging veins aren’t just cosmetic—they signal that your vein valves aren’t working properly. They may feel tender, heavy, or itchy.Sores or ulcers that are slow to heal
CVI can reduce oxygen delivery to the skin, especially around the ankles. This makes wounds stubborn, painful, and more prone to infection.
If you notice these signs, especially if they worsen over time, it’s a good idea to see a doctor. A painless ultrasound can help confirm if your veins are struggling and guide treatment options.
How to Prevent Chronic Venous Insufficiency Before It Starts
The good news? You don’t have to wait for symptoms to show up to take care of your veins. These simple, proactive steps can help prevent CVI—or at least slow its progression:
Get Moving Regularly
Sitting or standing for long periods can cause blood to pool in your legs. If you have a desk job or stand all day, make it a point to stretch or take a quick walk every hour. Even wiggling your toes or doing calf raises helps keep blood flowing.Maintain a Healthy Weight
Extra pounds increase the pressure on your leg veins, making it harder for blood to move upward. Keeping your weight in a healthy range reduces this stress and supports vein health.Elevate Your Legs Daily
Raising your legs above heart level for 15–20 minutes a day gives your veins a break and reduces pressure and swelling. It’s a simple habit with powerful benefits.Wear Compression Stockings (If Needed)
If you’re on your feet all day or have a family history of vein problems, compression stockings can be a great preventive tool. They support your veins and help push blood back toward your heart.Avoid Tight Clothing
Clothes that constrict your waist, groin, or legs can restrict blood flow. Choose looser-fitting, breathable options that won’t put extra pressure on your veins.Stay Hydrated and Eat a Vein-Friendly Diet
A diet rich in fiber, antioxidants, and low in salt helps prevent water retention and supports strong blood vessels. Drinking plenty of water also helps your circulation run smoothly.
Can You Treat Chronic Venous Insufficiency?
Yes—and the sooner, the better! Treatment options range from simple lifestyle changes to medical procedures, depending on the severity of your symptoms and how much your veins are affected.
Lifestyle Fixes That Help
Move more – Regular walking or leg exercises encourage healthy circulation.
Even light movement like ankle rolls or standing up every 30 minutes can prevent blood from pooling in your legs.Elevate your legs – Resting with your legs above heart level reduces swelling.
Try propping your legs up on pillows for 15–20 minutes a few times a day to relieve pressure and help blood flow back toward your heart.Wear compression stockings – These special socks gently squeeze your legs to help push blood upward.
They're available in various strengths and lengths—your doctor can recommend the right type for your needs.Maintain a healthy weight – Shedding extra pounds eases pressure on your veins.
Even modest weight loss can improve circulation and reduce symptoms like swelling and leg fatigue.
Medical Treatments
If symptoms are severe or not improving with lifestyle changes, your doctor may suggest one or more of these options:
Sclerotherapy – A solution is injected into problem veins to close them off.
Over time, the treated vein fades away and blood reroutes to healthier vessels. It’s often used for varicose or spider veins.Endovenous ablation – Uses heat or laser to seal off damaged veins.
This minimally invasive procedure is done under local anesthesia and has little downtime. It’s a popular choice for larger, problematic veins.Surgery – In rare cases, veins may be removed or repaired surgically.
This may be recommended for advanced CVI or when other treatments haven't worked. Options include vein stripping or bypass procedures.
Living Well With Chronic Venous Insufficiency
Chronic venous insufficiency may be a long-term condition, but with the right habits and care, you can stay active, comfortable, and in control of your health.
Stick to your routine – Whether it’s wearing compression stockings, doing daily leg exercises, or elevating your legs in the evening, consistency is key. Small daily actions can make a big difference in how your legs feel.
Check your skin regularly – Because chronic venous insufficiency (CVI) can lead to skin changes or even ulcers, keep an eye on your legs for new spots, dryness, or open sores. Moisturize daily and let your doctor know if anything looks unusual.
Don’t skip follow-ups – Regular check-ins with your healthcare provider help track your progress and make adjustments as needed. They may monitor circulation or suggest new treatments if symptoms change.
Keep moving, even a little – Walking, stretching, or low-impact activities like swimming keep blood flowing. If you work at a desk, set reminders to stand up and move around throughout the day.
Eat for vein health – A diet rich in fruits, vegetables, fiber, and water helps prevent constipation and supports circulation. Reduce salt intake to minimize swelling.
Protect your legs – Avoid sitting with legs crossed for long periods, wear supportive footwear, and be cautious with hot baths or heating pads, which can dilate veins further.
Living with chronic venous insufficiency doesn’t mean giving up your lifestyle—it just means being more mindful of your legs and circulation. With a proactive approach, many people manage their symptoms effectively and maintain a high quality of life.
Don’t Ignore the Warning Signs
Chronic venous insufficiency doesn’t go away on its own—and without treatment, it can lead to painful ulcers, blood clots, and permanent skin damage.
The good news? With the right care, most people get real relief and can avoid long-term complications. If your legs are trying to tell you something, it’s time to listen.
Final Thoughts
Chronic venous insufficiency (CVI) is more than just a cosmetic issue or minor nuisance. It’s a real medical condition that deserves attention. So, if you’re noticing swelling, aching, or bulging veins in your legs, don’t wait. Talk to your healthcare provider, start moving more, and show your veins some love.
Your legs work hard for you—let’s return the favor.
Sources:
Cleveland Clinic
https://my.clevelandclinic.org/health/diseases/16872-chronic-venous-insufficiency-cviMayo Clinic
https://www.mayoclinic.org/diseases-conditions/varicose-veins/symptoms-causes/syc-20350643American Heart Association
https://newsroom.heart.org/news/what-is-chronic-venous-insufficiencySociety for Vascular Surgery
https://vascular.org/your-vascular-health/vascular-conditions/chronic-venous-insufficiencyBMJ Best Practice
https://bestpractice.bmj.com/topics/en-us/507
Pulse Your Health
Empowering you to achieve your health goals.
Contact
© 2026. All rights reserved.
Disclaimer: The content on this website is for informational purposes only and is not medical advice. Always seek the advice of your physician or other suitably qualified healthcare professional for diagnosis, treatment and your health related needs.
