Stay updated on what is trending in health. Discover tips and resources for a healthier, balanced life.
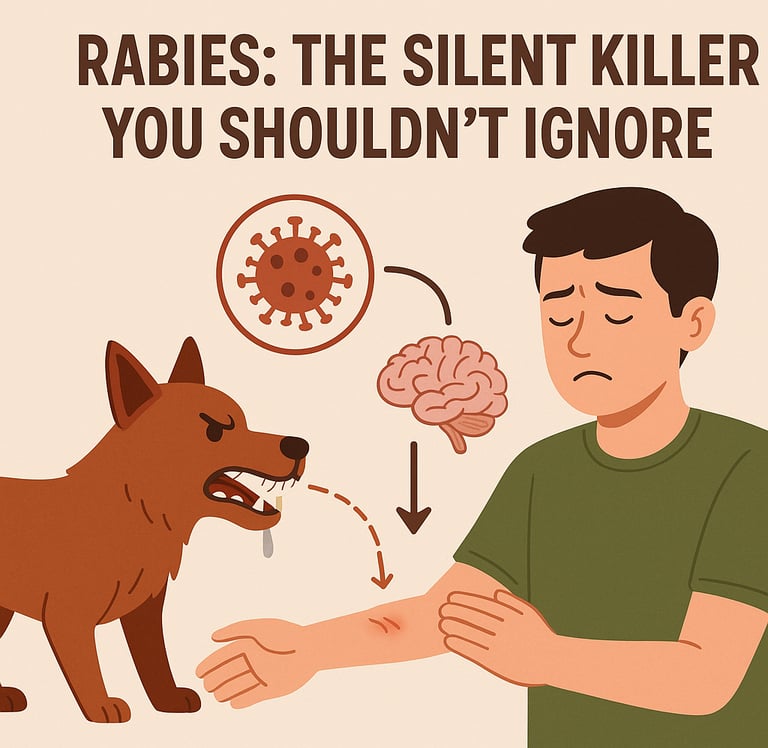
Rabies: The Silent Killer You Shouldn’t Ignore
Rabies is a deadly but preventable virus spread through animal bites. Learn how rabies spreads, its symptoms, prevention, and what to do after exposure in this clear, expert-backed guide.
DISEASES AND CONDITIONS
Dr. S. Ali
8/17/20257 min read
Rabies might sound like something out of an old horror story—a dog foaming at the mouth, behaving erratically, chasing after people. But the truth is, rabies is very real, very deadly, and sadly, still very common in many parts of the world. It doesn’t get the media attention of some other infectious diseases, but that doesn’t make it any less dangerous.
If you’ve ever been scratched or bitten by a dog, cat, or even a bat, you need to know the facts about this virus. Because when it comes to rabies, prevention is everything. Once symptoms appear, it’s almost always too late.
So let’s talk about what rabies really is, how it spreads, what symptoms to watch for, and how you can protect yourself and your family.
What Is Rabies, Exactly?
Rabies is a viral infection that targets the brain and nervous system. It’s caused by the rabies virus, which belongs to a group of viruses called Lyssaviruses. The virus is usually passed from animals to humans through a bite, and it travels from the site of the bite or scratch to the brain via the nerves.
What makes rabies so frightening is that it’s almost always fatal once symptoms start. But here’s the good news: it’s also almost 100 percent preventable if action is taken early enough.
How Do People Get Rabies?
Most human cases of rabies are caused by dog bites, especially in regions where stray dogs are common and vaccination coverage is low. But dogs aren't the only culprits. Other animals, including cats, bats, raccoons, skunks, and foxes, can also spread the virus.
Here’s how rabies can spread:
Bites from infected animals
This is the most common route. The rabies virus lives in the saliva of infected animals. When they bite and break the skin, the virus is introduced directly into the body.Scratches that break the skin
Even if an animal doesn’t bite, a scratch can still transmit the virus—especially if the animal's claws are contaminated with infected saliva. If the scratch breaks the skin, the virus can enter the bloodstream or nearby nerves.Licks on broken skin or mucous membranes
If an infected animal licks an open wound or areas like the eyes, nose, or mouth, the virus can find its way in through the moist surfaces or damaged tissue.
It’s important to note that rabies isn’t spread by casually petting an animal or touching its fur. You also can’t catch it from an animal’s urine or feces. The real danger comes when saliva from an infected animal gets into broken skin or mucous membranes like the eyes or mouth. That said, it’s never a good idea to try petting a wild, stray, or sick-looking animal—especially if it’s behaving strangely. Even if the risk from touch is low, an infected animal can bite or scratch without warning, and that’s where the real risk begins.
Once the virus enters the body, it doesn’t attack immediately. It travels slowly through the nerves toward the brain—a process known as the incubation period. This period typically lasts one to three months, but it can be shorter or much longer depending on factors like the location and severity of the bite. For example, bites closer to the head or neck tend to lead to quicker symptom onset.
The Incubation Period: A Dangerous Delay
One of the tricky things about rabies is that it doesn’t cause symptoms right away. After someone is bitten or scratched, the virus takes time to travel through the nerves toward the brain. This period—called the incubation period—can range from a few days to several months. The average is about one to three months.
This delay gives a false sense of security. A person might feel fine for weeks after the bite and assume they’re in the clear. But once the virus reaches the brain and symptoms appear, the chances of survival are incredibly slim.
That’s why post-exposure treatment needs to begin as soon as possible—ideally within a few hours after a bite.
Signs and Symptoms of Rabies
In the early stages, rabies can be sneaky. The symptoms often mimic the flu, so you might not realize something more serious is going on. But as the virus spreads to the brain, the signs become more severe and unmistakable.
Early symptoms may include:
Fever
A mild to moderate fever is often one of the first signs. It’s your body’s natural response to fighting off an infection, though it doesn’t specifically point to rabies.Headache
Many people develop a persistent headache. It may feel like general pressure or throbbing and is often dismissed as stress or dehydration in the early stages.Tiredness
Fatigue or a general feeling of being unwell is common. This can make it harder to notice more specific symptoms early on.Pain or tingling at the bite site
One of the more telling early signs is a strange sensation at the site of the bite or scratch. People often describe it as itching, burning, tingling, or pain—even if the wound appears healed. This is a red flag that the virus may be traveling along the nerves.
As the infection progresses and reaches the brain, symptoms become more severe:
Confusion or agitation
As the virus affects the central nervous system, people may become disoriented, irritable, or emotionally unstable. This may appear as unexplained restlessness, panic, or irrational behavior.Hallucinations
Some patients experience vivid hallucinations—seeing, hearing, or feeling things that aren't there. This is a sign that the brain is under severe stress and inflammation.Muscle spasms
Sudden, involuntary muscle contractions—particularly in the neck and throat—are common. These can become painful and interfere with normal movement or breathing.Difficulty swallowing
Rabies can cause severe throat muscle spasms, making it hard to swallow food, liquids, or even saliva. This leads to a choking sensation and contributes to the fear of water.Excess saliva or drooling
Because swallowing becomes difficult, saliva begins to build up. This can cause drooling, and in some cases, the classic image of foaming at the mouth.Fear of water (hydrophobia)
Despite extreme thirst, patients may develop an intense fear or aversion to drinking water. Just seeing or attempting to swallow water can trigger painful throat spasms. Hydrophobia is a unique and well-known sign of rabies.Paralysis
As the virus continues to spread in the brain and spinal cord, it may cause partial or total paralysis. This usually begins in the limbs and can progress to the respiratory muscles, leading to breathing failure.
Eventually, rabies causes the patient to fall into a coma, and without intensive life support, death usually follows within days. Once these advanced neurological symptoms appear, there is no effective treatment, which is why early intervention is critical.
How Is Rabies Diagnosed?
Rabies can be hard to diagnose in the early stages because the symptoms are so vague. There's no single test that can reliably detect rabies before symptoms begin. Diagnosis is usually based on the person’s history—whether they were bitten or scratched by an animal that may have been rabid.
Once symptoms start, doctors may perform tests on saliva, spinal fluid, or skin samples, but by then, treatment is no longer effective. That’s why rabies is considered a clinical diagnosis early on, and treatment is usually started based on suspicion alone rather than waiting for test results.
What Should You Do After a Bite or Scratch?
If you’re bitten or scratched by an animal—especially a stray or wild one—don’t wait to see if you develop symptoms. Immediate action can save your life.
Here’s what to do:
Wash the wound thoroughly with soap and running water for at least 15 minutes. This helps reduce the viral load at the wound site.
Disinfect the wound using iodine or alcohol-based solutions if available.
Seek medical help right away. A doctor will assess whether you need post-exposure prophylaxis (PEP).
What Is Post-Exposure Prophylaxis (PEP)?
PEP is the treatment given after a potential rabies exposure. It involves a series of rabies vaccinations, usually given over two weeks. In some cases, a person may also receive a dose of rabies immune globulin (RIG), which provides immediate protection while the body builds up its own antibodies.
If given promptly—ideally within 24 to 48 hours of exposure—PEP is almost 100 percent effective at preventing rabies.
The treatment is safe, widely used, and highly effective. But it needs to be started before symptoms appear. Once the virus reaches the brain, it’s too late.
Is There a Vaccine for Rabies?
Yes, there’s a vaccine that can prevent rabies. It’s used in two main situations:
Pre-exposure vaccination: This is recommended for people at higher risk, such as veterinarians, animal handlers, laboratory workers dealing with the virus, or travelers going to areas with high rabies risk. It involves a series of shots over a few weeks and offers long-term protection.
Post-exposure vaccination: Given after a bite or suspected exposure, as explained above.
The vaccine is safe and effective, but many people in high-risk regions still lack access to it. Improving access to rabies vaccines is one of the key strategies for reducing global deaths.
Why Rabies Is Still a Global Health Concern
Despite being completely preventable, rabies still kills an estimated 59,000 people every year—mostly in Asia and Africa. The vast majority of these deaths are in children under the age of 15.
The reason? Lack of awareness, limited access to vaccines, and the presence of large populations of unvaccinated dogs.
In many areas, people may not realize how serious a bite can be. They might wait too long to seek treatment or turn to traditional remedies instead of going to a clinic. By the time they recognize the signs, it’s too late.
Can Rabies Be Eradicated?
Technically, yes. Rabies can be eliminated through widespread dog vaccination, public education, and access to prompt medical care. Some countries have already eliminated rabies through national vaccination campaigns and strict pet control laws.
But in many low-resource settings, challenges like poverty, poor veterinary infrastructure, and misinformation still stand in the way.
Global health organizations, including the World Health Organization (WHO), aim to achieve zero human deaths from dog-mediated rabies by 2030. It's an ambitious but achievable goal.
Final Thoughts: What You Can Do
Rabies doesn’t have to be a death sentence. In fact, no one should die from rabies today. The tools for prevention are available—it’s just a matter of education, access, and quick action.
If you live in a region where rabies is present, stay informed and take it seriously. Get your pets vaccinated regularly, avoid contact with stray or wild animals, and teach children what to do if they’re bitten or scratched.
And if you ever think you might have been exposed, don’t wait. Go to a healthcare facility immediately. The sooner you act, the better your chances of staying safe.
When it comes to rabies, it’s always better to be cautious than to be sorry.
Sources:
World Health Organization (WHO) – Rabies Key Facts
https://www.who.int/news-room/fact-sheets/detail/rabies
Centers for Disease Control and Prevention (CDC) – Rabies
https://www.cdc.gov/rabies/index.html
World Organisation for Animal Health (WOAH) – Rabies
https://www.woah.org/en/disease/rabies/
Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/rabies/symptoms-causes/syc-20351821
Global Alliance for Rabies Control (GARC)
https://rabiesalliance.org/
Pulse Your Health
Empowering you to achieve your health goals.
Contact
© 2026. All rights reserved.
Disclaimer: The content on this website is for informational purposes only and is not medical advice. Always seek the advice of your physician or other suitably qualified healthcare professional for diagnosis, treatment and your health related needs.
