Stay updated on what is trending in health. Discover tips and resources for a healthier, balanced life.
Pancreatitis: What It Is, Why It Happens, and How to Heal
Understand pancreatitis, including acute, chronic, and necrotising pancreatitis—learn the causes like gallstones and alcohol, key symptoms, treatment options, prevention tips, and how diet and lifestyle changes can protect your pancreas and improve digestive health.
DISEASES AND CONDITIONS
Dr. S. Ali
5/2/20254 min read
If you have ever heard someone mention pancreatitis and thought, “Pancrea-what?”—you’re not alone. It’s not the most talked-about condition, but it should be. Pancreatitis is more common than you might think and can become serious if left untreated. But don't worry—let’s break it down in plain English and talk about what causes it, how it feels, and what you can do about it.
So, What Exactly Is Pancreatitis?
In simple terms, pancreatitis is inflammation of the pancreas—a small but powerful organ tucked behind your stomach. The pancreas has two big jobs: it helps you digest food and it regulates your blood sugar. When it gets inflamed, things go haywire.
There are two main types:
Acute pancreatitis – comes on suddenly and doesn’t last long. In severe cases, it can lead to necrotizing pancreatitis, where parts of the pancreas tissue die due to intense inflammation. This can be life-threatening and often requires urgent medical care.
Chronic pancreatitis – sticks around for a long time and can cause permanent damage, leading to digestive issues and even diabetes over time.
What Causes Pancreatitis?
Several things can trigger pancreatitis, but the two most common causes are:
Gallstones – tiny stones that form in your gallbladder and can block the bile duct, preventing pancreatic enzymes from draining properly. This backup causes irritation and inflammation in the pancreas, often leading to acute pancreatitis.
Heavy alcohol use – especially over time, can damage pancreatic tissue and interfere with normal enzyme function. Repeated alcohol-related inflammation increases the risk of chronic pancreatitis and serious complications like necrosis.
Other causes include:
High triglycerides – When fat levels in your blood skyrocket (especially over 1,000 mg/dL), it can trigger inflammation in the pancreas.
Certain medications – Some drugs like diuretics, corticosteroids, and certain antibiotics can irritate the pancreas in rare cases, especially when used long-term or in high doses.
Smoking – Tobacco use damages pancreatic tissue and increases your risk of both acute and chronic pancreatitis, even if you don’t drink alcohol.
Abdominal injuries – Trauma from car accidents, falls, or surgery can physically harm the pancreas and lead to inflammation.
Infections – Viral infections like mumps, hepatitis, or Epstein-Barr virus can sometimes inflame the pancreas as part of a broader illness.
Autoimmune conditions – In autoimmune pancreatitis, the body’s immune system mistakenly attacks the pancreas, causing swelling and tissue damage.
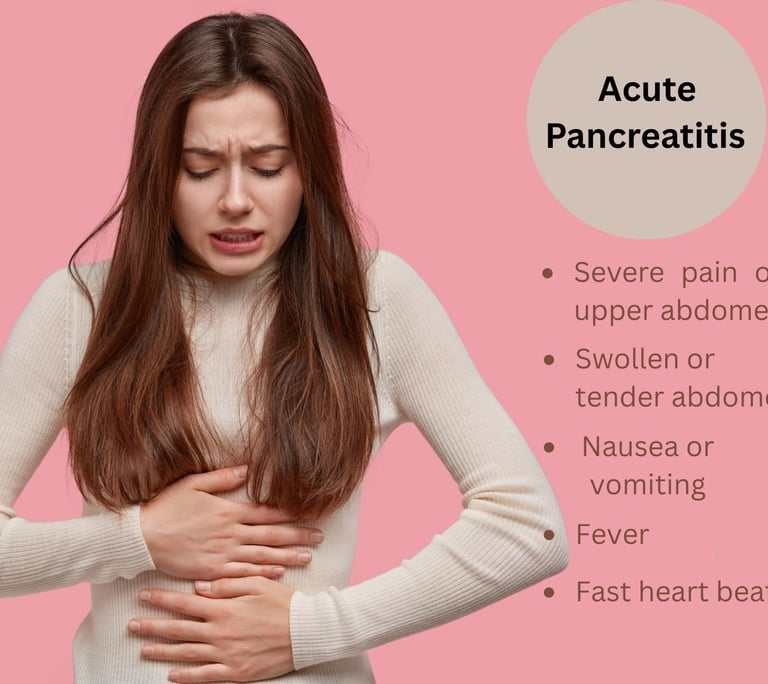
What Does Pancreatitis Feel Like?
People usually describe it as a sudden, sharp pain in the upper belly, often radiating to the back. Some other symptoms include:
Nausea or vomiting
Fever
Swollen or tender abdomen
Fast heartbeat
If it’s chronic, you might also lose weight (without trying) or have oily, smelly stools due to poor digestion.
If you ever feel intense belly pain that won’t go away—don’t wait. Seek medical help ASAP (as soon as possible).
How Is It Treated?
Treatment depends on how severe it is. For mild cases, the main goals are to let the pancreas rest and reduce inflammation. This often means:
No food or drink for a while (yes, really—your pancreas needs a break)
IV fluids to keep you hydrated
Pain relief and treatment for the underlying cause
If it’s caused by gallstones, you might need surgery. If alcohol is the culprit, quitting is essential to avoid future flare-ups.
For chronic pancreatitis, treatment also includes enzyme supplements to help you digest food and sometimes insulin if blood sugar becomes an issue.
Can You Prevent Pancreatitis?
Absolutely. Here’s how:
It starts with a few smart lifestyle choices. While some risk factors (like genetics or autoimmune conditions) are out of your hands, many causes of pancreatitis are totally preventable.
1. Limit alcohol—or avoid it altogether
Excessive drinking is one of the biggest risk factors for both acute and chronic pancreatitis. If you've had pancreatitis before, it's best to steer clear of alcohol completely.
2. Eat a healthy, low-fat diet
High-fat meals can trigger flare-ups, especially if you have gallstones. Focus on whole foods—like fruits, veggies, lean proteins, and whole grains. Think grilled salmon, steamed greens, oats, and avocado—not greasy fast food.
3. Avoid smoking
Smoking increases the risk of pancreatic inflammation and also makes recovery harder. If you smoke, quitting is one of the best things you can do for your pancreas (and your whole body).
4. Manage triglyceride levels and diabetes
High triglycerides can lead to acute pancreatitis, while uncontrolled blood sugar levels stress your pancreas. Regular check-ups, medication if needed, and healthy eating can help keep both in check.
5. Stay hydrated and maintain a healthy weight
Drinking enough water supports digestion and overall organ health. And maintaining a healthy weight reduces your risk of gallstones and metabolic disorders—both linked to pancreatitis.
Taking care of your pancreas isn't complicated—it just takes a bit of awareness and consistency. Treat your gut well, and it will return the favor.
Your pancreas will thank you!
Final Thoughts
Pancreatitis might sound scary, but knowing what causes it and how to treat it can make a big difference. If you suspect you have it, listen to your body and get medical advice early. And even if you’re healthy now, a few simple lifestyle tweaks can go a long way toward protecting your pancreas.
Keep an eye on your belly—because your gut health is more powerful than you think.
Sources:
National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Pancreatitis
https://www.niddk.nih.gov/health-information/digestive-diseases/pancreatitisMayo Clinic – Pancreatitis
https://www.mayoclinic.org/diseases-conditions/pancreatitisCleveland Clinic – Pancreatitis
https://my.clevelandclinic.org/health/diseases/10236-pancreatitis
BMJ Journals Banks PA, Bollen TL, Dervenis C, et al.
Classification of acute pancreatitis—2012: revision of the Atlanta classification and definitions by international consensus. Gut. 2013;62(1):102–111.
https://gut.bmj.com/content/62/1/102American Gastroenterological Association (AGA) Clinical Guidelines
https://www.gastro.org/guidelines
Pulse Your Health
Empowering you to achieve your health goals.
Contact
© 2026. All rights reserved.
Disclaimer: The content on this website is for informational purposes only and is not medical advice. Always seek the advice of your physician or other suitably qualified healthcare professional for diagnosis, treatment and your health related needs.
