Stay updated on what is trending in health. Discover tips and resources for a healthier, balanced life.
Left Ventricular Assist Devices (LVAD) or the “Heart Pump”
Learn about Left Ventricular Assist Devices (LVAD): how they work, who needs them, benefits, risks, and future innovations. A guide to heart pump technology.
HEALTHCARE SERVICES
Dr. S. Ali
9/5/20256 min read
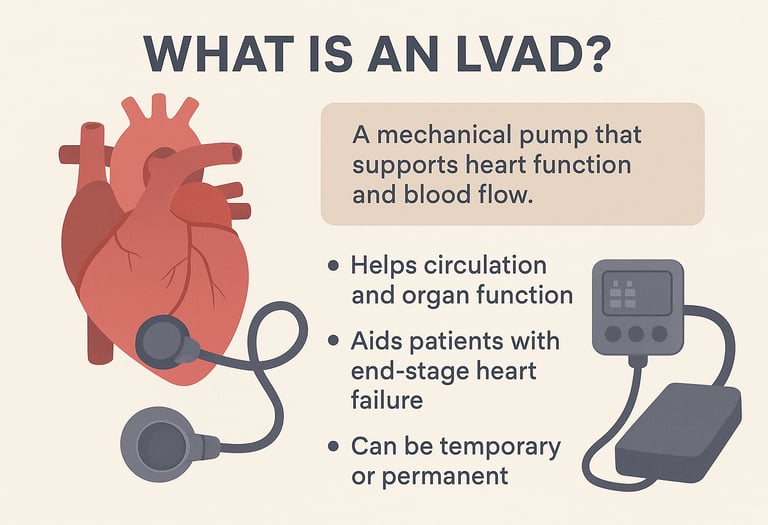
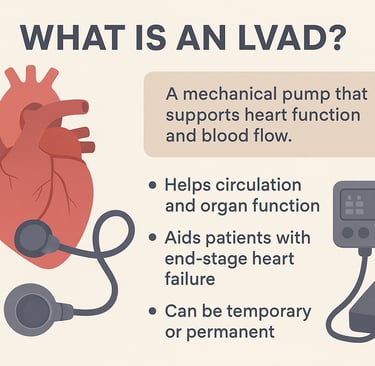
What is an LVAD?
A Left Ventricular Assist Device (LVAD) is a mechanical pump that helps a weak heart circulate blood. It’s most often used in people with advanced heart failure who no longer respond to standard treatments. By taking over part of the left ventricle’s job, the LVAD allows oxygen-rich blood to flow through the body more effectively.
Doctors may recommend an LVAD for conditions like cardiomyopathy, severe valve disease, or as a bridge while waiting for a heart transplant. For some patients who can’t get a transplant, it can also serve as long-term therapy. Many people experience less fatigue and shortness of breath, better exercise tolerance, and an overall improved quality of life with an LVAD.
How Does an LVAD Work?
An LVAD is implanted surgically and connected to the left ventricle and the aorta. The pump draws blood from the heart and pushes it into the aorta, ensuring that circulation continues even when the heart is too weak to do the job alone.
The device has a pump inside the chest and a controller with batteries outside the body. Most modern LVADs use continuous flow, creating a steady stream of blood rather than a pulse, which explains why some patients may not have a detectable pulse.
By improving blood flow and oxygen delivery, the LVAD reduces symptoms like shortness of breath and allows patients to regain strength while awaiting transplant—or even live with it long term.
Who Needs an LVAD?
LVADs are usually recommended for people with severe heart failure (often New York Heart Association class III or IV) who still struggle with symptoms despite medication and lifestyle changes. Common causes include ischemic heart disease, cardiomyopathy, or valve disease.
They are often used as a bridge to transplant for patients awaiting a donor heart. In others, they can be used as destination therapy, offering long-term support when transplantation isn’t an option.
In short, an LVAD is not just a device—it’s a lifeline for people whose hearts are too weak to keep up with the body’s needs.
The LVAD Implantation Process
Getting an LVAD is a major surgery that starts with careful preparation. Doctors review your medical history, run tests to check your heart function, and discuss the risks, benefits, and lifestyle changes that come with the device.
During surgery, patients are placed under general anesthesia. The surgeon makes an incision in the chest, places the pump inside the left ventricle, and connects it to the aorta so blood can flow efficiently through the body. The device is then linked to an external controller and power source.
After surgery, patients spend time in the ICU for close monitoring. This recovery phase is when patients and families learn how to care for the driveline, watch for signs of infection or device issues, and adjust to life with the LVAD.
Living with an LVAD
Life with an LVAD requires daily care and some lifestyle changes. Patients must check batteries, keep the driveline clean and secure, and follow good hygiene to lower infection risk.
Certain activities, especially contact sports or anything that risks injury, are discouraged. Instead, light exercises like walking and stretching are encouraged to stay healthy. Exercise plans are usually customized with guidance from the healthcare team.
Regular follow-up visits are essential to monitor the heart, medications, and device performance. Patients also learn to spot warning signs like unusual weight changes, blood pressure shifts, or redness around the driveline. With the right care and adjustments, many people live active, fulfilling lives with an LVAD.
Benefits of an LVAD
An LVAD can be life-changing for people with advanced heart failure.
By helping the heart pump more effectively, it improves circulation so that vital organs like the brain, kidneys, and liver get the oxygen and nutrients they need. This not only helps the body function better day-to-day but also prevents further complications from poor blood flow.
Many patients notice a dramatic reduction in symptoms such as constant fatigue, swelling in the legs, and shortness of breath. With these symptoms under better control, everyday activities—like walking around the house, climbing stairs, or even enjoying hobbies—become easier again.
Another major benefit is extended survival. For patients whose outlook would otherwise be very limited, an LVAD can add months or even years of life, allowing more time with family and friends.
Finally, the device provides hope for those awaiting a heart transplant. It serves as a bridge, keeping patients stable and strong enough to undergo transplant surgery when a suitable donor heart becomes available. For others who are not transplant candidates, it can still be used as long-term therapy, offering a second chance at living more fully. Many patients report that after getting an LVAD, they can walk farther, sleep better, and spend more quality time with loved ones.
Potential Risks and Complications
While LVADs can be life-changing, they also come with some risks.
The biggest concern is infection, since the device involves both surgery and an external driveline. Careful hygiene and regular monitoring are essential to keep infections under control.
Another risk is pump malfunction or power failure, though this is rare. Patients are trained to recognize alarms, swap batteries, and contact their healthcare team quickly if problems arise.
Blood clots are also a concern, since the device changes how blood flows. Clots can lead to stroke or other complications, which is why most patients need blood thinners and regular check-ups to keep clotting levels safe.
By staying on top of these risks with good habits and medical support, most people live well with an LVAD.
The Future of LVAD Technology
LVAD technology is advancing rapidly, making devices smaller, safer, and easier to live with. Newer pumps are more compact, which means less invasive surgery and quicker recovery. Researchers are also developing biocompatible materials that lower infection risk and extend device durability.
Another exciting step is the use of remote monitoring and telemedicine, allowing doctors to track patients’ devices in real time and intervene early if something goes wrong.
The future points to lighter, more user-friendly LVADs that blend into daily life, offering heart failure patients more freedom, comfort, and peace of mind.
LVAD vs. Heart Transplant: What’s the Difference?
An LVAD doesn’t replace your heart—it works alongside it. Think of it as a mechanical helper that takes over some of the pumping work so your heart doesn’t have to struggle as much. For some people, an LVAD is used as a temporary solution while waiting for a donor heart. For others, especially those who may not be transplant candidates, it becomes a long-term or even permanent therapy that allows them to live with better quality of life.
A heart transplant, on the other hand, completely replaces your failing heart with a healthy donor heart. This can be a life-saving option, but it comes with its own challenges, such as the need for lifelong medications to prevent the body from rejecting the new organ.
In many cases, patients may start with an LVAD as a “bridge to transplant,” giving them the strength and stability they need until a donor heart becomes available. In other cases, the LVAD itself becomes the final therapy, especially if a transplant isn’t possible.
FAQs About LVADs
1. Can you live a normal life with an LVAD?
Yes! Many people return to work, travel, and enjoy hobbies, though it requires adjustments.
2. How long can someone live with an LVAD?
Modern devices can last 5 years or more, with some patients living even longer.
3. Will I feel the pump inside me?
You won’t feel the pump working, but you may notice the driveline and equipment at first.
4. Can you shower with an LVAD?
Direct water is not safe for the device. Most patients use special shower kits to stay clean.
5. Does the LVAD cure heart failure?
No, it manages symptoms and improves quality of life but doesn’t cure the underlying disease.
Conclusion
An LVAD can feel intimidating at first, but for many patients, it’s truly life-changing. It provides the heart with the extra push it needs, relieves symptoms, and gives people the chance to live fuller lives.
If you or someone you love is considering an LVAD, talk to your healthcare team about whether it’s the right step. With the right support and knowledge, life with an LVAD can be not only possible but fulfilling.
Related Articles:
Sources:
American Heart Association (AHA) – Heart Failure and LVADs
https://www.heart.org/en/health-topics/heart-failure/treatment-options-for-heart-failure/ventricular-assist-devicesNational Heart, Lung, and Blood Institute (NHLBI) – LVAD Overview
https://www.nhlbi.nih.gov/health/ventricular-assist-deviceCleveland Clinic – LVAD: What It Is & How It Works
https://my.clevelandclinic.org/health/treatments/17086-ventricular-assist-devicesJohns Hopkins Medicine – Ventricular Assist Device Therapy
https://www.hopkinsmedicine.org/heart-vascular-institute/cardiology/heart-failure/ventricular-assist-deviceMayo Clinic – Ventricular Assist Devices
https://www.mayoclinic.org/tests-procedures/ventricular-assist-device/about/pac-20384976American Society of Transplantation – LVADs and Transplant Bridge Therapy
https://www.myast.org/patient-information/ventricular-assist-device
Pulse Your Health
Empowering you to achieve your health goals.
Contact
© 2026. All rights reserved.
Disclaimer: The content on this website is for informational purposes only and is not medical advice. Always seek the advice of your physician or other suitably qualified healthcare professional for diagnosis, treatment and your health related needs.
