Stay updated on what is trending in health. Discover tips and resources for a healthier, balanced life.
Idiopathic Pulmonary Fibrosis (IPF): What You Need to Know About This Silent Lung Disease
Learn what idiopathic pulmonary fibrosis (IPF) is, its symptoms, causes, and treatment options. This progressive lung disease can be tricky to spot—early diagnosis matters.
DISEASES AND CONDITIONS
Dr. S. Ali
7/27/20255 min read
What Is Idiopathic Pulmonary Fibrosis?
Let’s break it down.
“Idiopathic” means we don’t know exactly what causes it.
“Pulmonary” refers to the lungs.
“Fibrosis” means scarring.
So, idiopathic pulmonary fibrosis—or IPF—is a chronic lung disease where scar tissue builds up in the lungs over time, making it harder to breathe. This scarring gets worse gradually, and unlike regular tissue, scar tissue can’t heal or work the same way. Over time, the lungs stiffen and lose their ability to transfer oxygen into the bloodstream effectively.
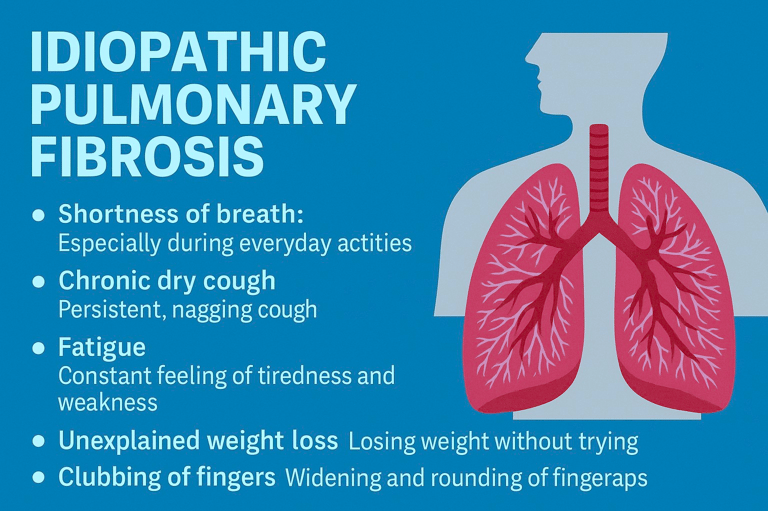
What Are the Symptoms of IPF?
The tricky part? Symptoms often start out mild and are easy to brush off. Many people assume they’re just out of shape or recovering from a cold. But here’s what to look for:
Shortness of breath:
Especially during everyday activities like walking or climbing stairs. At first, it might only show up when you're exerting yourself—but as the disease progresses, you may feel breathless even while sitting still. Many people mistake this for just being “out of shape.”Chronic dry cough:
A persistent, hacking cough that sticks around for months, not linked to a cold, allergies, or other infections. It often worsens over time and can be frustratingly disruptive during conversations, sleep, or meals.Fatigue:
You may feel constantly tired, even after a full night’s sleep. The reduced oxygen supply to your body can leave you drained, making everyday tasks feel exhausting.Unexplained weight loss:
Some people lose weight without trying, often due to the body working harder to breathe and chronic inflammation. It may be gradual or sudden, and is easy to overlook if you’re not actively tracking your weight.Clubbing of fingers:
The tips of your fingers become rounder, softer, and wider—a classic sign of long-term low oxygen levels. This change happens slowly and is usually painless, so it’s often spotted by a doctor during a physical exam.
Over time, breathing can become more and more difficult, even while at rest.
What Causes IPF?
Here’s the frustrating part: we don’t really know. That’s what “idiopathic” means.
However, experts believe a few factors may increase the risk:
Age:
It usually affects people over 50. IPF rarely shows up in younger adults, and the risk increases as you get older—especially past age 60.Smoking:
A history of smoking raises your risk. Even if you quit years ago, past tobacco use is strongly linked to lung scarring and inflammation associated with IPF.Environmental exposures:
Long-term exposure to dust, fumes, or certain chemicals—such as silica, asbestos, or metal dust—can irritate the lungs and increase your risk. Jobs in farming, construction, or mining may carry higher exposure.Genetics:
In some cases, it runs in families. If you have a close relative with IPF or a related lung disease, your risk may be higher due to inherited gene mutations.Viral infections:
Some viruses may play a role in triggering the disease. Researchers have linked IPF to chronic infections like Epstein-Barr virus (EBV), hepatitis C, and certain herpes viruses.
How Is IPF Diagnosed?
IPF can be hard to diagnose because the symptoms overlap with other lung conditions like asthma, COPD, or even heart disease.
Your doctor may recommend:
Chest X-rays or high-resolution CT scans
These imaging tests help detect patterns of lung scarring typical of IPF. A high-resolution CT scan is especially useful for showing fine details that may not appear on a standard X-ray.Pulmonary function tests
These measure how much air your lungs can hold and how well you can move air in and out. Reduced lung capacity and stiff lungs are common signs of IPF.Blood tests
Blood work can help rule out autoimmune diseases or other causes of lung inflammation. While they can’t diagnose IPF directly, they’re important for narrowing down the possibilities.Lung biopsy (in some cases)
If imaging and other tests aren’t conclusive, a small sample of lung tissue may be taken. This allows doctors to look at the cells under a microscope to confirm IPF or check for other lung diseases.
Seeing a pulmonologist (lung specialist) is often necessary for a clear diagnosis.
Is There a Cure?
Unfortunately, there’s no cure for IPF yet, but treatments can help slow the progression and manage symptoms.
Here’s what’s available:
Anti-fibrotic medications
Drugs used for the treatment of IPF don’t cure IPF, but they can slow the progression of lung scarring and preserve lung function for as long as possible. Starting treatment early may help preserve lung function for longer and improve quality of life.Oxygen therapy
Supplemental oxygen helps maintain healthy oxygen levels in your blood, especially during physical activity or sleep. It can ease shortness of breath and reduce fatigue so you can keep doing the things you enjoy.Pulmonary rehabilitation
This is more than just exercise—it’s a tailored program that combines physical training, breathing techniques, and education. It helps boost stamina, improve mood, and empower you to manage your condition better.Lung transplant
For people with advanced IPF who meet specific criteria, a lung transplant may offer a chance at longer survival. It’s a big decision that involves careful evaluation, but for some, it’s the best hope for a better future.
What’s the Outlook?
IPF is a progressive disease, meaning it worsens over time. The rate of progression varies—some people remain stable for years, while others decline more rapidly.
But here’s the key: early diagnosis and treatment can make a big difference. Managing your lifestyle, staying active, avoiding infections, and sticking to treatment can help improve your quality of life.
Living With IPF: Tips That Help
Here’s how to support your lungs every day:
Avoid smoking and secondhand smoke
Tobacco smoke can worsen lung damage and speed up disease progression. Quitting smoking (and avoiding smoky environments) is one of the most important steps you can take to protect your lungs.Get vaccinated against flu, pneumonia, and COVID-19 to avoid infections
Lung infections can hit harder when you have IPF. Staying up to date with your vaccines lowers your risk of serious illness and helps keep your lungs working as well as possible.Eat well and stay hydrated
Nutritious meals give your body the energy it needs to fight inflammation and stay strong. Small, frequent meals may be easier to manage if shortness of breath affects your appetite.Join a support group—talking to others with IPF can help you feel less alone
Connecting with others who truly understand your journey can provide emotional relief, share practical tips, and remind you that you’re not facing this condition on your own.Monitor your symptoms and report any changes to your doctor
If your cough worsens, breathing gets harder, or you notice new symptoms, don’t wait. Catching problems early can help your doctor adjust your care plan before things get worse.
Final Thoughts
Idiopathic Pulmonary Fibrosis might be a mouthful, but awareness is everything. The more we know about this condition, the sooner we can spot it—and take action.
If you or someone you know has been experiencing unexplained shortness of breath or a chronic cough, don’t ignore it. A conversation with your doctor could be the first step toward better breathing.
Sources:
American Lung Association
https://www.lung.org/lung-health-diseases/lung-disease-lookup/idiopathic-pulmonary-fibrosis
National Heart, Lung, and Blood Institute (NHLBI)
https://www.nhlbi.nih.gov/health/idiopathic-pulmonary-fibrosis
Pulmonary Fibrosis Foundation (PFF)
https://www.pulmonaryfibrosis.org
Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/idiopathic-pulmonary-fibrosis
MedlinePlus (U.S. National Library of Medicine)
https://medlineplus.gov/idiopathicpulmonaryfibrosis.html
Pulse Your Health
Empowering you to achieve your health goals.
Contact
© 2026. All rights reserved.
Disclaimer: The content on this website is for informational purposes only and is not medical advice. Always seek the advice of your physician or other suitably qualified healthcare professional for diagnosis, treatment and your health related needs.
