Flesh-Eating Bacteria: What You Need to Know About This Rare but Deadly Infection
Flesh-eating bacteria, or necrotizing fasciitis, is a rare but deadly infection. Learn the causes, symptoms, and how to protect yourself from this fast-moving condition.
DISEASES AND CONDITIONS
Dr. S. Ali
7/17/20256 min read

You've probably heard the term “flesh-eating bacteria” on the news or social media—and it sounds terrifying, doesn’t it? While the name is dramatic, the infection it refers to is very real and can be life-threatening if not treated quickly.
So, what is flesh-eating bacteria? Who’s at risk? And how can you protect yourself? Let’s break it down in plain language.
What Is Flesh-Eating Bacteria?
"Flesh-eating bacteria" is the nickname for a serious condition called necrotizing fasciitis. It happens when certain bacteria infect the deeper layers of skin and tissue, spreading rapidly and destroying everything in their path.
Despite the scary name, this condition is rare—but it requires immediate medical attention. Without fast treatment, it can cause permanent damage or even be fatal.
What Causes It?
Several types of bacteria can cause necrotizing fasciitis, but the most common culprit is:
Group A Streptococcus (GAS) – the same bacteria that cause strep throat.
→ These bacteria can rapidly invade tissues and produce toxins that destroy skin, fat, and muscle.
Other possible bacteria include:
Clostridium
→ Known for causing gas gangrene, these bacteria thrive in low-oxygen environments and produce toxins that damage tissue.Klebsiella
→ This bacterium can cause severe soft tissue infections, especially in people with weakened immune systems or chronic illnesses.Escherichia coli (E. coli)
→ While some strains are harmless, others can cause serious infections when they enter the body through wounds.Staphylococcus aureus, including MRSA
→ These bacteria are often resistant to antibiotics and can cause aggressive skin and tissue infections.Vibrio vulnificus
→ Found in warm seawater, this bacterium can enter through open wounds or be ingested via raw seafood, leading to rapid tissue destruction.
These bacteria can enter the body through a cut, scrape, insect bite, surgical wound, or even a minor bruise. Once inside, they spread quickly along tissue planes and release toxins that kill tissue and interfere with blood flow.
Real-World Case: Florida Deaths Highlight Rising Risk
In July 2025, Florida confirmed four deaths linked to flesh-eating bacteria—Vibrio vulnificus—along with a total of eleven infections statewide. All cases involved individuals who had open wounds exposed to warm coastal waters or consumed raw shellfish. These tragic events underscore how rapidly necrotizing fasciitis can progress—within hours—and why early medical intervention is crucial. Health officials now strongly advise covering any cuts before entering the water and promptly seeking care at the first sign of infection.
Early Warning Signs: What to Watch For
This infection starts fast and gets worse even faster. That’s why early recognition is critical. Here are symptoms to watch for:
Severe pain that feels worse than the injury looks
This is often the first red flag. If the pain keeps increasing despite the wound appearing minor, it could signal deep tissue damage.Redness or swelling that spreads quickly
Infections that expand rapidly within hours may mean bacteria are spreading beneath the skin—don’t ignore it.Skin that feels warm or hard
Heat and firmness around the area are signs your immune system is fighting something serious below the surface.Fever, chills, or dizziness
These systemic symptoms suggest the infection has entered your bloodstream and is affecting your whole body.Blisters, black spots, or purple patches
Discolored or blistered skin means tissue is dying—get to the ER right away if you see these changes.Nausea or confusion as the infection worsens
As toxins spread, your body may react with confusion, vomiting, or disorientation—urgent signs of sepsis.
If you ever notice pain that feels “out of proportion” to a small cut or injury—don’t wait. Seek medical help immediately.
Who’s Most at Risk?
Necrotizing fasciitis can affect anyone, but some people are more vulnerable, including:
People with diabetes
High blood sugar can weaken the immune system and reduce circulation, making it harder for the body to fight infections and heal wounds.Those with weakened immune systems
Conditions like HIV/AIDS or medications such as steroids and chemotherapy reduce the body’s defenses against aggressive bacteria.Cancer patients or organ transplant recipients
Treatments like chemotherapy or anti-rejection drugs suppress immunity, increasing the risk of life-threatening infections from minor injuries.People with chronic illnesses (like kidney or liver disease)
These conditions can impair your immune function and slow healing, allowing infections to take hold more easily.Individuals with open wounds, recent surgery, or trauma
Breaks in the skin—no matter how small—can be entry points for bacteria. Surgical wounds and injuries are especially vulnerable if not kept clean.IV drug users
Using non-sterile needles or injecting in unsanitary conditions greatly increases the risk of skin and soft tissue infections, including necrotizing fasciitis.
Even healthy people can get it, especially if exposed to warm, salty water or through contaminated wounds. Open cuts, insect bites, or scrapes at the beach or in floodwaters can be dangerous if harmful bacteria are present.
How Is It Treated?
Treatment needs to be fast and aggressive. It usually includes:
High-dose IV antibiotics These are the frontline defense against infection, delivered directly into the bloodstream for maximum impact. The goal is to halt the spread of bacteria quickly before it causes further damage.
Emergency surgery to remove infected tissue Surgical intervention may be needed to eliminate necrotic or abscessed areas. This helps stop the infection at its source and prevents it from compromising nearby healthy tissue.
In severe cases, multiple surgeries or even amputation When infections are deep or widespread, repeated procedures may be necessary. In extreme cases, amputation can be life-saving by removing irreparably damaged areas and preventing systemic infection.
Supportive care in an intensive care unit (ICU) Critical care teams provide around-the-clock monitoring, fluid management, respiratory support, and other vital interventions. The ICU environment helps stabilize patients and manage complications like sepsis or organ failure.
Early diagnosis improves survival rates dramatically. Delay can lead to septic shock, organ failure, or death.
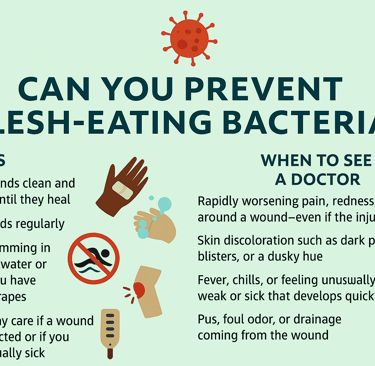
Can You Prevent Flesh-Eating Bacteria?
Yes—while it’s rare, there are smart steps you can take to lower your risk:
Keep wounds clean and covered until they heal This helps block bacteria from entering vulnerable areas. Use antiseptic solutions and change bandages regularly to minimize infection risk.
Wash hands regularly Hand hygiene is your frontline defense against many infections. Scrubbing with soap for at least 20 seconds is especially important before touching wounds.
Avoid swimming in warm saltwater or lakes if you have cuts or scrapes Warm, brackish water can harbor harmful bacteria like Vibrio. Even small skin openings can provide an entry point—so sit out the swim if you're not fully healed.
Don’t delay care if a wound looks infected or if you feel unusually sick Redness, swelling, fever, or increasing pain could be early signs of a serious infection. Swift medical attention can be life-saving.
Manage chronic conditions like diabetes carefully Conditions that impair circulation or immune response can make infections harder to fight. Keeping blood sugar in check and monitoring skin health reduces your vulnerability.
When to See a Doctor
Early intervention can save lives when it comes to flesh-eating bacteria and other serious skin infections. Seek medical care immediately if you notice:
Rapidly worsening pain, redness, or swelling around a wound—even if the injury seems minor This can indicate fast-spreading infection and tissue damage, which may require immediate surgical intervention.
Skin discoloration such as dark patches, blisters, or a dusky hue These signs suggest compromised blood flow or necrosis, often associated with severe bacterial infection.
Fever, chills, or feeling unusually weak or sick that develops quickly Systemic symptoms like these can mean the infection is affecting internal organs or leading to sepsis.
Pus, foul odor, or drainage coming from the wound These are red flags for bacterial growth and tissue breakdown—and should never be ignored.
Loss of sensation or increasing pain, which may indicate tissue damage Numbness or deep, burning pain can be early signs of necrotizing fasciitis and require emergency evaluation.
If symptoms escalate fast or spread beyond the injury site, don’t wait. Go to the nearest emergency room or urgent care center. Better safe than sorry.
The Bottom Line
Flesh-eating bacteria may sound like something out of a horror movie, but the real-life condition—necrotizing fasciitis—is a medical emergency that requires fast action. Fortunately, it’s rare. The key is knowing the signs, protecting your skin, and seeking medical care without delay if something feels off.
Your best defense? Good hygiene, wound care, and not ignoring red flags.
Sources:
Centers for Disease Control and Prevention (CDC)
https://www.cdc.gov/vibrio/index.html
Mayo Clinic
https://www.mayoclinic.org/diseases-conditions/necrotizing-fasciitis/symptoms-causes/syc-20354771
World Health Organization (WHO) – General Infectious Disease Info https://www.who.int/health-topics/infectious-diseases
Singapore Food Agency (SFA) – Necrotising Fasciitis Overview
https://www.sfa.gov.sg/food-safety-tips/food-risk-concerns/risk-at-a-glance/necrotising-fasciitis-(flesh-eating-disease)
Florida Department of Health (FDOH)
https://www.floridahealth.gov
USA TODAY – Vibrio vulnificus deaths in Florida
https://www.usatoday.com/story/news/health/2025/07/15/flesh-eating-bacteria-vibro-vulnificus-deaths-florida/85209349007/
CBS News Miami – Florida Vibrio vulnificus cases and deaths
https://www.cbsnews.com/miami/news/florida-vibrio-vulnificus-cases-2025-deaths-decline-danger-remains/
WUSF Public Media – Florida Health Department Report
https://www.wusf.org/health-news-florida/2025-07-15/flesh-eating-bacteria-leads-to-four-deaths-in-florida-this-year-health-department-reports
