Stay updated on what is trending in health. Discover tips and resources for a healthier, balanced life.
Ankylosing Spondylitis: Symptoms, Causes, and Treatment
Learn about ankylosing spondylitis: causes, symptoms, diagnosis and treatment. Discover the lifestyle changes needed and how to cope with this disease and live a healthy life.
DISEASES AND CONDITIONS
Dr. S. Ali
2/28/20253 min read
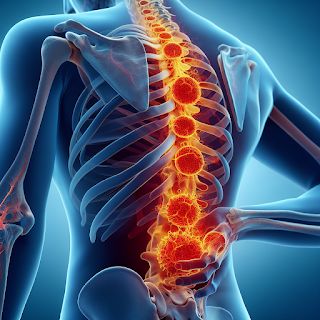
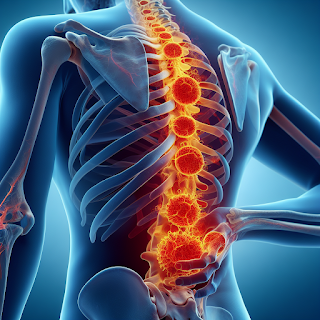
Ankylosing Spondylitis: Causes, Symptoms, and Treatment Options
Ankylosing spondylitis (AS) is a chronic inflammatory arthritis that primarily affects the spine, causing inflammation, stiffness, and fusion of the vertebrae. Ankylosing Spondylitis can also impact other joints and organs like the eyes, heart, lungs, and kidneys. This autoimmune disease often leads to a hunched posture and reduced flexibility.
What is Ankylosing Spondylitis?
Ankylosing spondylitis is an autoimmune disorder that causes chronic inflammation in the joints of the spine. Over time, this can lead to fusion of the vertebrae, resulting in limited mobility and flexibility. Ankylosing Spondylitis typically begins in the lower back (sacroiliac joints) and gradually spreads to the upper spine. It can also affect other joints such as the hips and shoulders, as well as other organs.
Causes of Ankylosing Spondylitis
The exact cause of Ankylosing Spondylitis is unclear, but it is believed to be triggered by a combination of genetic and environmental factors. The gene HLA-B27 plays a significant role, but not everyone with this gene develops Ankylosing Spondylitis. Other triggers include infections, physical trauma, smoking, and hormonal changes.
Symptoms of Ankylosing Spondylitis
Symptoms of ankylosing spondylitis can vary greatly from person to person. While some may experience only mild discomfort, others may face more severe symptoms that limit daily activities. The hallmark signs of ankylosing spondylitis include:
Chronic back pain: This pain typically persists for more than three months and is often felt in the lower back and buttocks. The pain tends to improve with movement.
Morning stiffness: Stiffness in the spine and joints is common, especially after periods of inactivity (such as waking up in the morning or sitting for extended periods).
Reduced flexibility: Over time, the inflammation may reduce the range of motion in the spine and other affected joints.
Fatigue: Many people with Ankylosing Spondylitis experience chronic fatigue, which can significantly impact daily functioning.
Swelling in other joints: Ankylosing Spondylitis can affect joints beyond the spine, including the hips, knees, and shoulders.
Eye inflammation: A condition known as uveitis (inflammation of the eye) is common in people with ankylosing spondylitis.
Diagnosis of Ankylosing Spondylitis
Diagnosing ankylosing spondylitis involves a combination of medical history review, physical examination, blood tests, and imaging studies. There is no single test to confirm Ankylosing Spondylitis, so doctors rely on various diagnostic methods, including:
Medical History: Your doctor will ask about your symptoms, such as their duration, frequency, and severity. Family history and environmental triggers are also important to consider, as Ankylosing Spondylitis often runs in families.
Physical Examination: During the exam, your doctor will assess your posture, spine mobility, and the presence of joint inflammation or deformities.
Blood Tests: Blood tests can help identify markers of inflammation (such as C-reactive protein and erythrocyte sedimentation rate). Additionally, the HLA-B27 gene test may be conducted, although it is not definitive for diagnosing Ankylosing Spondylitis.
Imaging Tests: X-rays, MRI scans, and CT scans are used to evaluate the condition of the sacroiliac joints, spine, and other affected areas. In the early stages of Ankylosing Spondylitis, changes in the joints may not be visible, so imaging tests are used alongside clinical evaluation.
Treatment for Ankylosing Spondylitis
While there is no cure for Ankylosing Spondylitis, several treatment options can help manage symptoms and improve quality of life:
Medications:
NSAIDs to reduce pain and inflammation.
DMARDs (Disease-modifying antirheumatic drugs) for severe cases.
Biologic drugs to target specific inflammatory molecules.
Corticosteroids for short-term flare-ups.
Physical Therapy: Helps improve posture, flexibility, and strength, and prevents spinal deformities.
Surgery: In severe cases, surgery such as joint replacement or spinal fusion may be necessary.
Lifestyle Modifications:
Quit smoking to reduce inflammation.
Regular exercise to maintain flexibility and mobility.
Healthy diet rich in anti-inflammatory foods.
Stress management techniques like prayer, yoga and meditation.
Living with Ankylosing Spondylitis
Although Ankylosing Spondylitis is a chronic condition, lifestyle changes and proper treatment can significantly improve quality of life. Regular exercise, healthy eating, stress management, and proper medication can help manage symptoms and prevent progression of the disease.
Conclusion
Ankylosing spondylitis is a chronic condition that requires long-term management. While there is no cure, early diagnosis and appropriate treatment can help control inflammation, reduce pain, and prevent further joint damage. By taking an active role in managing symptoms through medication, physical therapy, and lifestyle modifications, individuals with ankylosing spondylitis can lead a fulfilling life. If you suspect you have Ankylosing Spondylitis, consult with a healthcare professional for proper evaluation and treatment.
Sources:
National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) - Ankylosing Spondylitis Overview
Mayo Clinic - Ankylosing Spondylitis Symptoms and Causes
Spondylitis Association of America (SAA) - What is Ankylosing Spondylitis?
Arthritis Foundation - Ankylosing Spondylitis Treatment and Management
Pulse Your Health
Empowering you to achieve your health goals.
Contact
© 2026. All rights reserved.
Disclaimer: The content on this website is for informational purposes only and is not medical advice. Always seek the advice of your physician or other suitably qualified healthcare professional for diagnosis, treatment and your health related needs.
